Rectal Prolapse Treatment
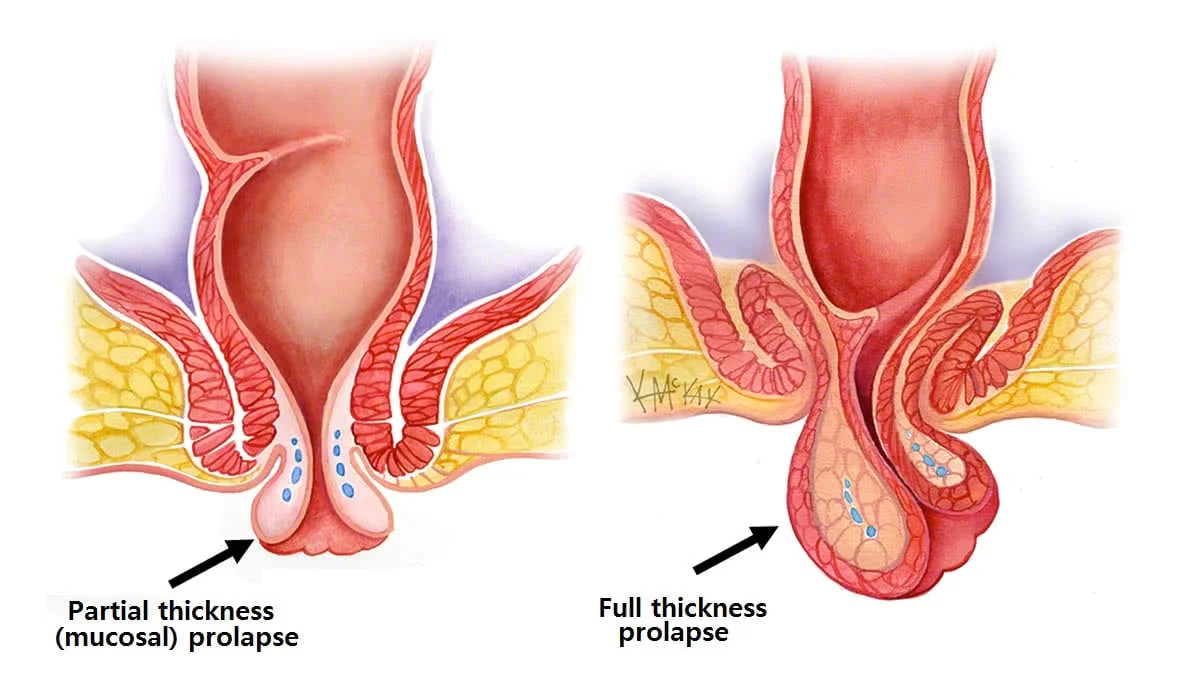
Rectal prolapse occurs when the rectum (the last part of the large intestine) slips or protrudes through the anus. It can be partial or complete and is more common in elderly individuals, women after childbirth, or people with chronic constipation or weakened pelvic muscles.
Treatment varies depending on the severity, age, general health, and whether the prolapse is internal or external.
1. Diagnosis Services
-
Physical Examination: To identify visible prolapse or protrusion during straining.
-
Rectal Exam: To assess tone and muscle strength.
-
Colonoscopy or Sigmoidoscopy: To rule out tumors, polyps, or other bowel conditions.
-
Defecography (X-ray or MRI): To see how the rectum moves during bowel movements.
-
Manometry: Measures rectal pressure and sphincter function (for chronic cases).
2. Non-Surgical Management
Recommended only for very early-stage or internal prolapse (rectal intussusception) without severe symptoms:
-
Dietary Modifications: High-fiber foods and hydration to prevent straining.
-
Stool Softeners or Laxatives: To ease bowel movements.
-
Pelvic Floor Therapy / Kegel Exercises: To strengthen anal and rectal muscles.
-
Biofeedback Therapy: For patients with rectal dysfunction or chronic constipation.
?? Non-surgical treatments only manage symptoms—they do not cure rectal prolapse.
3. Surgical Treatment Services
Surgery is the definitive treatment for most moderate to severe rectal prolapse cases.
a. Rectopexy (Abdominal Surgery)
-
The rectum is repositioned and secured inside the pelvis using sutures or mesh.
-
Can be done via laparoscopic (keyhole) or open surgery.
-
Often combined with resection (removal of a redundant colon segment) if constipation is a major symptom.
b. Perineal Procedures (for elderly or high-risk patients)
-
Done through the anus, no abdominal incision required.
-
Altemeier Procedure (Perineal Rectosigmoidectomy): The prolapsed rectum is removed through the anus.
-
Delorme Procedure: Inner lining of the rectum is removed and outer muscle tightened.
-
Less invasive but higher recurrence rate compared to rectopexy.
c. Laparoscopic or Robotic-Assisted Surgery
-
Advanced and minimally invasive options
-
Less postoperative pain, faster recovery
-
Preferred for younger and healthier patients
4. Post-Surgical Care Services
-
Wound care and pain management
-
Constipation prevention and bowel training
-
Pelvic floor physiotherapy
-
Dietary and lifestyle counseling
-
Regular follow-up appointments to check for recurrence or complications
5. Additional Hospital Services May Include
-
Pre-surgical fitness and anesthesia evaluation
-
Day-care admission for laparoscopic surgeries
-
Cashless insurance and claim processing
-
Private recovery rooms
-
Online follow-up consultations
-
24/7 emergency surgical team availability
